Meniscus Tear
What is the Meniscus?
The knee Joints are lined by extremely smooth tissue called “articular cartilage.”
The articular cartilage of the knee coats
- The end of the femur (thigh bone),
- The top surface of the tibia (shin bone) and
- The back surface of the patella (kneecap)
In addition each knee has two menisci (cartilages); on the
- Inner side (medial meniscus)
- Outer side (lateral meniscus).
The meniscus’ role is to:
- Reduce wear
- Protect against arthritis
- Assist with stability of the knee joint, and
- Help disperse fluid around the knee joint effectively.
What is a Meniscal Tear?
Meniscal tears are commonly occurring cartilage injuries. Meniscus tears can be painful and debilitating.
The meniscus is an important structure of the knee, and damage to the meniscus can lead to osteoarthritis of the knee in the long term.
Causes of Meniscal Tears
Meniscal tears can be either
Degenerative - occur as part of the aging process due to progressive wear or as a result of habitual, prolonged squatting.
Sometimes no trauma is required as the meniscus stiffens and weakens with age.
Meniscus tears are a special risk for older athletes and more than 40% of active patients 65 or older have them.
Traumatic - occur in the athletic setting
The meniscal cartilage is at risk of tearing due to constant exposure to repetitive loading as we walk, run or perform other activities.
Where the knee is partially bent under load or involved in twisting motions (pivoting during sports, squatting, heavy lifting and changing direction) the meniscus can tear under pressure.
Higher risk sports include:
- Football
- Basketball
- Soccer
- Tennis
Meniscal tears can also occur in combination with tears of ligaments around the knee (eg an ACL tear).
Symptoms of a Meniscal Tear?
Meniscal tears have the following symptoms
- Knee pain
- Swelling within 24 hours
- Difficulty walking for several days.
While these acute symptoms can resolve spontaneously, other prolonged symptoms can include:
- Loss of full range of motion
- Inability to either bend or fully straighten the knee
- Pain with walking
- Tenderness along the joint line
- A tendency for your knee to get "stuck" or lock up
- Audible ‘clicking’
Painful instability may be present and this can be difficult to distinguish from instability resulting from an ACL rupture.
Meniscal Tear Diagnosis
Dr Biggs will need to diagnose the specific nature of the torn meniscus or the extent of any osteoarthritis in the knee joint
Often, meniscus damage can be identified during a physical examination..
During this consultation Dr Biggs will:
- Take a medical history
- Perform a physical examination
- Assess the joint’s range of motion
Imaging tests:
- X-rays do not show cartlidge but are often normal as they can help rule out other problems with the knee that may have similar symptoms like fractures (broken bone) or ACL injury.
- MRI can create detailed images of both hard and soft tissues within your knee. An MRI can produce cross-sectional images of internal structures required if the diagnosis is unclear or if other soft tissue injuries are suspected such ligament injuries or articular cartilage injuries.
While not all of these tests are required to confirm the diagnosis, this diagnostic process will allow Dr Biggs to review any possible risks or existing conditions that could interfere with the surgery or its outcome.
Arthroscopy
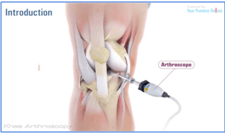
In some cases, Dr Biggs may need to perform a procedure known as an arthroscopy. This is necessary if the exact cause of the pain is not clear.
What is an Arthroscopy
Arthroscopy is a surgical procedure in which an arthroscope is inserted into a joint.
An arthroscope is a device that Dr Biggs uses to see inside your knee joint. It includes a tiny camera at its tip.
If necessary, surgical instruments can be inserted through the arthroscope or through additional small incisions in your knee.
The benefits of arthroscopy include
- Small incisions
- Fast healing
- Rapid recovery and
- Little scarring.
Arthroscopic surgical procedures can be performed on an outpatient basis. This means patients can return home the same day of the procedure.
Arthroscopy of the Knee Joint
Knee arthroscopy is an operation that involves inserting a small camera into your knee. The camera sends an image of the inside of your knee to a screen. Instruments are inserted into the knee through a second small incision at the front of the knee.
The benefits of arthroscopy include
- Smaller incisions
- Faster healing
- More rapid recovery and
- Less scarring
Some arthroscopic surgical procedures can be performed on an outpatient basis. This means patients can return home the same day of the procedure.
Risks With Knee Arthroscopy?
Complications are not common but can occur.
Prior to making any decision to have surgery, it is important that you understand the potential risks so that you can make an informed decision regarding the advantages and disadvantages of surgery.
The following list is by no means exhaustive, so it is important to discuss your concerns with Dr Biggs.
General surgical risks include:
- Risk of infection
- Postoperative bleeding
- Clotting in the leg (deep vein thrombosis - DVT) or lung.
Apart from surgical risks, medical (including allergies) and anaesthetic complications can occur, and these can affect your general well being and health.
Knee Arthroscopy - Patient Info Handouts
![]() Click here to download the PDF
Click here to download the PDF
Treatment for a Meniscal Tear?
Unfortunately, meniscal tears do not heal without surgery.
Not everyone requires surgery and treatment is tailored to the patient’s individual needs. The less active patient may be able to return to a quieter lifestyle without surgery
Surgery is advocated for patients less than 25 years old who are active especially if the tear is “fresh” (ie. less than 3 months), repairable and associated with an ACL injury.
While most meniscal tears are not repairable (ie. cannot be sutured back together), the removal of the torn portion only (ie. partial meniscectomy) and leaving the unaffected meniscus remnant is a surgical option. The result of this procedure can be a stable knee.
Surgery is recommended where patients endure ongoing episodes of
- Pain,
- Instability
- Swelling and
- Locking
Non surgical treatment involves physical therapy and rehabilitation to strengthen the quadriceps and hamstrings muscles to stabilise the knee and maintain range of movement.
Meniscal Surgery
Patients will usually require arthroscopic surgery to restore function and stability if wishing to return to:
- Sports involving cutting or pivoting movements (e.g. soccer, football and netball, etc.) or
- Physical jobs involving cutting or pivoting movements (eg. policeman, fireman, builders, etc)
Risks with Meniscal Surgery
Complications are not common but can occur. Prior to making any decision to have surgery, it is important that you understand the potential risks so that you can make an informed decision regarding the advantages and disadvantages of surgery.
The following list is by no means exhaustive, so it is important to discuss your concerns with Dr Biggs.
- Joint stiffness
- Local nerve or blood vessel damage
- There are small nerves under the skin that cannot be avoided and cutting them may lead to areas of numbness in the front of the knee. This area of numbness normally reduces in size with time and does not cause any functional problems with the knee. Very rarely there can be damage to important nerves in the leg.
- Reflex sympathetic dystrophy, while rare this condition is not entirely understood but can cause unexplained and excessive pain and stiffness after surgery or after a trivial injury
Preparing for Meniscal Repair Surgery
Once Dr Biggs decides that surgery is required, preparation is necessary to achieve the best results and a quick problem free recovery.
Preparing mentally and physically for surgery is an important step toward a successful result.
- Dr Biggs will create a treatment plan and
- Patients will also need to understand the process and their role in it
Dr Biggs will also need to:
- Discuss any medications being taken with your doctor or physician to see which ones should be stopped before surgery
- Do not eat or drink anything, including water, for 6 hours before surgery
- Stop taking aspirin, warfarin, anti-inflammatory medications or drugs that increase the risk of bleeding one week before surgery to minimise bleeding
- Review blood replacement options (including banking blood) with your doctor
- Consider alternate medical interventions and other treatments
- Eat a well-balanced diet, supplemented by a daily multivitamin with iron.
- Consider losing weight (if overweight) before surgery to help decrease the stress on the new joint. However, dieting one month before surgery.
- Stop or cut down smoking to reduce your surgery risks and improve your recovery
- Treat any tooth, gum, bladder or bowel problems before surgery to reduce the risk of infection
Report any infections to Dr Biggs prior to surgery as the procedure cannot be performed until all infections have cleared up.
After Your Operation:
Some patients need one night in hospital, although for most patients it is possible to leave hospital the day of surgery.
After your operation you will have pain medication and antibiotics.
The wounds take 7-10 days to heal. Most patients improve dramatically in the first 2 weeks.
Occasionally, there are periods where the knee may become sore and then settle again. This is part of the normal healing process. If a meniscal repair was performed, it can take 3 months for it to heal fully.
Full weight-bearing and walking is allowed immediately after a meniscectomy. Initially this will be aided by crutches, but once you regain strength and mobility the crutches can be discarded.
If a meniscal repair is performed, a period of protected weight-bearing may be required.
If any postoperative problems arise with your knee, such as redness, increasing pain or fevers, do not hesitate to contact Dr Biggs. If unavailable, seek advice from the hospital or your doctor.
When can I Drive After Meniscal Surgery?
Driving a car is discouraged for 48 hours after an anaesthetic. After 48 hours, your ability to drive will depend on the side you had your operation, left or right, and the type of vehicle you drive, manual or automatic. You can drive whenever you feel comfortable.
Return to Work After Meniscal Surgery
Return to work will vary depending on the procedure performed and type of work you do. Most patients can return to office work within 1 week. Labour intensive work however, may require up to 3 weeks before returning to full duties.
During this period patients are not fit to perform work duties that involve:
- Prolonged standing
- Heavy lifting
- Bending or
- Excessive stair climbing
Return to Sport After Meniscal Surgery
Activities or sports can be restarted after the wounds have healed, the postoperative swelling has subsided and range of movement is restored.
This usually takes 2-3 weeks following a meniscectomy alone. If a meniscal repair was performed, it is best to delay leisure activities or sports for 12 weeks to allow the meniscus time to heal and repair.
Pain Management
Often there is little pain after surgery. This is because local anaesthetic is injected around the wound during the procedure and it is performed arthroscopically (ie. minimally invasive keyhole surgery).